Lantus and Levemir are long-acting insulins (or basal insulins) that provide the background insulin needed to supply cells with glucose around the clock, while preventing the release of excess glucose from the liver and excess fat from fat cells. The waking glucose level best measures the activity of these insulins. All Type 1s and many Type 2s also require faster-acting insulin (such as Humalog, Novolog, or Apidra) to cover meals and lower high glucose levels. Some Type 2s who have adequate insulin production do well with one of these long-acting insulins, in combination with oral medications or a daily or weekly injection of a GLP-1 agonist.
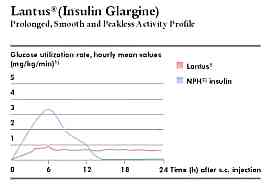
Lantus insulin (glargine), manufactured by Sanofi-Aventis, is promoted as a once-daily background insulin. However, many users find that it does not last a full 24 hours for them, and these users often notice a peak in activity about 6-8 hours after the injection. If once a day injection is giving you good control, there is no need to change and a bedtime injection is typically best. For others, splitting the dose and injecting twice a day (usually at breakfast and bedtime) often works better, lessens peaks and gaps in activity, and helps those who cannot inject Lantus within one hour of the same time each day. Lantus is slightly acidic and some may notice slight discomfort at the injection site.
Levemir insulin (detemir), manufactured by Novo Nordisk, works for approximately 18 hours and may experience a peak in activity 4-6 hours after injection. It is taken twice a day. Different people react to each insulin differently. The best advice is to try the other insulin if one does not seem to be working well for you.
Both basal insulins generally work quite well; however, neither can be mixed in a syringe with fast-acting insulin, and neither should be used in an insulin pump. Keep in mind that an older insulin called NPH can also provide very good results. NPH is less expensive, has a shorter action time, and is generally taken 3 times a day. One advantage of NPH is that it can be mixed in the same syringe with one of the rapid-acting insulins. Humalog, Novolog, or Apidra is loaded into the syringe first, then the NPH, and the injection is given right away. With its shorter action time and more peaking, NPH is sometimes helpful to address a need for more or less insulin action at a particular time of day, such as afternoon sports practices or a morning Dawn Phenomenon.
New insulins with action times measured in days rather than hours are being developed. These insulins appear to offer a slight reduction in the risk of hypoglycemia when taken once a day and greater convenience.
Tips For Starting
- Morning or night? Aventis recommends taking Lantus at bedtime, while Novo Nordisk recommends taking Levemir once or twice daily. Lantus’ actual duration of action is 18 to 26 hours, while Levemir is generally less than 22 hours. Although the timing of an insulin varies from person to person, it appears to be consistent in the same individual. One advantage of bedtime dosing is that if the insulin’s activity does not last 24 hours, the gap in activity typically occurs after dinner and can be covered with an extra injection of Humalog, Novolog, or Apidra at dinner.
- Consistent timing of the injection is crucial if it is administered once a day, so choose a time when you will remember to take the injection at the same time each day.
- The best way to eliminate gaps in insulin delivery when the insulin’s duration of action is less than 24 hours or when the timing of injections is erratic is to split the dose into two equal injections a day at breakfast and either dinner or bedtime. This helps smooth out the uneven insulin levels that often occur with once-daily dosing.
- Lantus and Levemir are clear insulins. Although the bottles have a different shape, some users have mistakenly injected a bedtime dose of fast-acting insulin instead of Lantus or Levemir. Be very careful not to confuse these long-acting insulins with your fast-acting clear insulin.
- Lantus becomes inactivated if it comes in contact with even small amounts of other insulins. This makes it appear hazy, so never use Lantus that is not crystal clear.
How Do I Know When I’m On The Right Dose?
One particularly beneficial feature of these insulins is that they make it easier to determine the correct dose. Because of the very stable 24-hour action when a sufficient number of doses are given, the dose(s) is gradually increased until the fasting or before breakfast blood sugar has been normalized. If low blood sugars occur during the night and are not being caused by a dose of fast-acting insulin taken during the evening hours, the dose(s) of long-acting insulin would be gradually reduced until the lows stop.
Similar to the basal rate of an insulin pump, Lantus and Levemir doses can be checked by skipping a meal during the day. The best test for determining whether the dose is accurate comes from stable, flat overnight blood sugar levels.
Once the Lantus dose has been determined, the doses of pre-meal Humalog, Novolog, or Type 2 medications would then be adjusted to keep post-meal blood sugars normal. With a stable background insulin level, carb counting becomes especially helpful in determining how much fast-acting insulin to take before each meal.
How Lantus Works
This insulin analog was designed to have low solubility in water at neutral pH, similar to that found in body fluids and other insulins. Lantus becomes completely soluble only at an acid pH of 4. Once this is injected under the skin, the acidic solution is neutralized, resulting in the formation of microprecipitates. The micro-precipitates enable the slow release of small amounts of insulin. This release results in a relatively constant concentration/time profile over 22 hours +/- 4 hours with a minimal peak in activity. Those who experience a shorter action time, such as 18 or 20 hours, will also experience more peaking activity about 6 hours following the injection.
Human insulin consists of two protein chains, designated as A and B, which are linked by two zinc cross-links between them. Lantus differs in that the amino acid asparagine at position A21 of the A chain is replaced by glycine, and two arginine molecules are added to one end of the B chain.
Cautions
Occasionally, the acidic nature of this insulin may cause mild discomfort at the injection site in some individuals. This does not appear severe enough to cause users to discontinue using Lantus insulin.
Like Humalog, Lantus is structurally different from human insulin, but it appears to cause an immune or allergic response rarely. Like any insulin allergy, the response can range from mild local itching to a severe allergic reaction with swelling of the tongue, inability to breathe, and shock or death if rapid treatment is not found.
Lantus should be used with caution and only under the supervision of a physician during pregnancy or prior to becoming pregnant.
The vast majority of users get consistent action from this insulin every day. However, Aventis’ clinical studies did identify some individuals who exhibited marked differences in the action time of Lantus from one day to the next. In rare individuals, its action time was as short as 11 hours; however, the reason for this difference is unknown.
How Levemir Works
Compared to human insulin, the last amino acid threonine in the B chain at B30 is clipped off in Levemir, and a short fatty acid is attached to the amino acid lysine at B29. The structural change causes 98% of the Levemir molecules to strongly bind to albumin, a protein in the blood, thereby providing Levemir with a prolonged action time. Some peaking occurs between 4 and 12 hours after an injection, but in most individuals, its activity levels out over time when administered twice a day. This insulin analog has no acidity and is soluble at a neutral pH of 7.4.
Lantus or Levemir may not work for everyone, but for the vast majority, one or two daily injections can provide outstanding results.
