Many people with Type 1 and Type 2 diabetes have high glucose levels and excess weight that makes them more susceptible to contracting a Covid-19 infection. More importantly, these place them at substantially higher risk for worse outcomes when infected. Poorly managed diabetes, excess weight, high blood pressure, and cardiovascular disease all promote chronic inflammation and oxidation that hinder immune responses. Higher glucose levels also impede oxygen delivery through organs and blood vessels they have previously damaged. For these reasons, diabetes and these associated issues significantly worsen outcomes with Covid-19. Fortunately, you can improve these in different ways. Your age is the only unmodifiable risk you face.
Well-managed glucose levels reduce the risk of catching COVID and ensure healthier outcomes if you do. See Pumping Insulin, 6th Edition, and Using Insulin for thorough information on managing glucose levels using a pump or injections. Our Insulin Dose Guide provides additional guidance.
COVID-19 Ain’t the Common Seasonal Flu!
Visit “Covid-19 Ain’t the Common Seasonal Flu! ” for details on how COVID-19 works and potentially becomes a severe threat and for Special Suggestions on Handling COVID-19 with Diabetes.
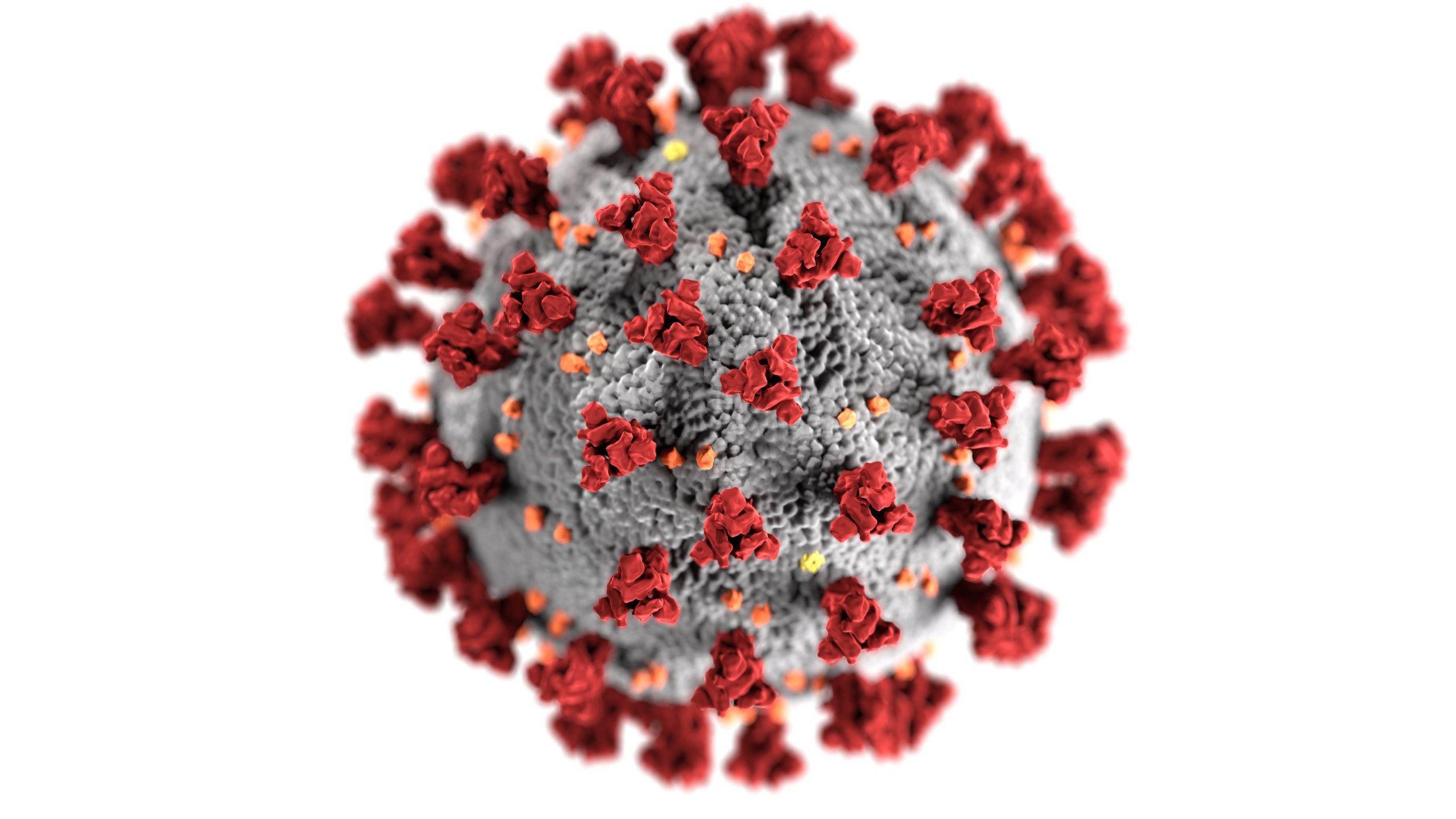
How an Infection Starts
First, let’s examine how to overcome COVID-19 and how it gets into cells and makes people sick. Infection begins when a protein enzyme in the human body alters and activates numerous spike proteins that extend from the outer wall of the virus. Once changed, these spikes attach to ACE2 (angiotensin-converting enzyme 2) enzymes. These enzymes reside on the exterior walls of cells in the nose, mouth, lungs, heart, kidneys, intestines, brain, and nerves. Their presence on multiple cells explains why COVID-19 can infect and impact many body organs.
Children have fewer and less severe infections, partly because they have fewer ACE2 entry points in their cells. Age, high blood pressure, and diabetes all increase the number of ACE2 receptors on cell walls. The virus gains virulence as people age, especially those with other medical issues.
Importance of the Renin-Angiotensin System
Among its tricks, COVID-19 throws the renin-angiotensin system(RAS) out of balance. RAS is responsible for maintaining a balance in the human body’s blood pressure and inflammatory systems. This balance lets you stand up from a lying position without fainting. It also enables you to increase inflammation to fight infection and decrease inflammation once you have dealt with it. A healthy balance in these inflammatory processes is essential for health.
The first RAS pathway, involving ACE, Angiotensin II, AT1 receptors, and aldosterone, raises blood pressure and inflammation. A second RAS pathway involving ACE2 (a different ACE enzyme), angiotensin 1-7, and a Mas receptor decreases these processes.
High glucose levels, excess weight, kidney disease, high blood pressure, and heart disease often coexist with diabetes. Each independently generates excess oxidation and inflammation raises pro-inflammatory cytokine levels and impairs immune responses. Diabetes preloads the COVID-19 viral cannon with far more gunpowder compared to otherwise healthy individuals.
The chronic inflammation seen with poorly controlled diabetes and its cofactors activates the first inflammatory RAS pathway. When COVID-19 enters this scene, it attaches to ACE2 and inactivates the second anti-inflammatory pathway. This double whammy magnifies potentially fatal increases in blood pressure and inflammation, narrows blood vessels, and increases clotting. Diabetes and its cofactors increase threats for severe outcomes, including hospitalization and intubation with COVID-19.
Anyone with higher glucose levels (A1c over 7%), an elevated microalbumin-to-creatinine level (over 30 mg/g), a fatty liver (elevated ALT or AST levels), or insulin resistance (low HDL cholesterol) has a high likelihood of having leaky blood vessels and cardiovascular disease. Vascular leakage makes it more likely that excess fluid will build up in the tiny alveoli of the lungs, block oxygen uptake, and hinder the release of carbon dioxide. With COVID-19, breathing can quickly become labored, often described as breathing with an elephant on your chest.
ACE Inhibitors and ARBs
Two classes of blood pressure medications, ACE inhibitors and ARBs, reduce blood pressure and inflammation by how they impact the first RAS pathway. ACE inhibitors, like lisinopril and enalapril, block the formation of angiotensin II. Working on a different path, angiotensin II receptor blockers or ARBs, like losartan, prevent the formation of aldosterone.
Typically used to treat hypertension, heart failure, and chronic kidney disease, these medications are now being studied to determine if they offer protection against organ damage in COVID-19. Alternatively, they might worsen the infection by increasing the number of ACE receptors, allowing more viruses to enter cells. Research suggests ACE and ARB blood pressure medications play a protective role rather than worsen the infection. More data is needed.
Covid-19 rapidly worsens the already elevated inflammation in diabetes. The virus can directly damage the insulin beta cells, causing glucose levels to rise. Rapid and significant increases in insulin doses are then required to control these glucose levels, even in some with no prior history of diabetes.
Cytokines and the Immune System
A healthy and robust immune system is essential for a successful counter-attack. Inflammation with the production and release of cytokines is an early immune system response to the virus. The formation of antibodies that the immune system uses to target the spike protein for a more precise attack by macrophages that destroy Covid-19 takes longer. Antibody production takes about ten days for the human body to develop fully and 2 to 3 weeks to reach maximal levels.
Cytokines are a two-edged sword, necessary to fight an infection but deadly to the host if their release becomes excessive. An excessive viral load or any delay in immune response due to excess weight, lack of exercise, or high glucose levels magnifies the initial inflammatory response. Raising the danger, COVID-19 directly delays the attack by anti-inflammatory interferons while promoting the overproduction of other pro-inflammatory interferons.
A lack of balance in the immune response can throw the body into a cytokine storm before an adequate antibody response begins. Scientists report that an inexpensive steroid medication, dexamethasone, can significantly reduce the cytokine storm and mortality in people with a severe infection. Numerous other anti-inflammatory agents are currently being studied in research studies in search of an anti-inflammatory cocktail that uses dexamethasone and other agents to minimize uncontrolled inflammation and deaths.
Fever and other symptoms of this virus mainly result from the release of cytokines. An extreme, uncontrolled release of cytokines promotes inflammation that necessitates intubation and ventilation in an ICU.
COVID-19 triggers responses from over 40 different cytokines. These include interferon gamma-induced protein 10 (IP-10), monocyte-chemotactic protein 3 (MCP3 or CCL7), C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-alpha), interleukin-6 (IL-6), IL-2, IL-7, IL-8, and IL-10. The inflammation that follows can generate widespread cell damage with a higher risk of cell death. Only a clinical lab evaluation can determine the degree and danger of an immune response. Early reports based on minimal data suggested that OTC anti-inflammatory medications might cause harm. However, both ibuprofen and naproxen are now in clinical trials to evaluate potential benefits against Covid-19.
Steps to Take with High Blood Pressure or Heart Disease
Dr. Eric Adler, a cardiologist at the University of California, San Diego, stresses how high blood pressure and vascular disease worsen outcomes with COVID-19. Both are more common with diabetes. Because COVID-19 attacks the lungs and is frequently associated with bacterial pneumonia, bacterial infections frequently occur, increasing demands on the heart and blood vessels as oxygen delivery plummets. The situation can worsen when fever promotes a rapid heart rate or arrhythmia.
Dr. Alder warns, “Those with heart issues need more oxygen, and when they are sick with a cold or virus, such as COVID-19, this need for oxygen greatly increases chances for severe complications, including the risk of stroke.”
What To Do If You Have High Blood Pressure or Heart Disease
Dr. Adler suggests that people with high blood pressure or heart disease follow these five tips:
- Protect yourself. Follow the guidelines given by your health care provider and do everything you can to prevent contracting COVID-19. Practice social distancing, shelter in place at home, avoid public places as much as possible, and wear a mask when in public.
- Contact your healthcare provider immediately if you get sick or develop symptoms related to COVID-19, such as fever, shortness of breath, or a new cough.
- Stay on your medications for heart disease and hypertension.
- Listen to your body. Do not ignore symptoms that may indicate heart disease or a stroke, such as chest pain or tightness, shortness of breath, numbness, or confusion. For people at high risk, chest pain could signal a heart attack. Do not delay treatment if you are worried.
- Eat well and exercise daily. Eat a balanced diet, avoid stress, and exercise for at least 30 minutes daily.
Diseases such as heart failure or cancer do not wait for Covid-19 to subside. Dr. Adler says it is crucial to maintain good health and continue to receive life-saving treatments.
Other Steps to Lower Your Risk and Live a Fuller Life:
During the months and perhaps years it will take to get the virus under control, here are additional things you can do to avoid and fight COVID-19. They apply to everyone but are especially helpful with diabetes.
- Check the health of your community. When positive tests stay below 5% for two weeks, adequate testing is conducted to keep viral transmission under control. Crossing paths with the virus becomes less likely. The closer the number is to 2%, the better.
- Limit the number of close contacts – Choose your bubble. You are safest with members of your household.
- Manage your exposure ‘budget.’ During a pandemic, every member of your home should manage their exposure budget. Budget points are lower for choices like a once-a-week grocery trip or exercising outdoors. You spend more budget points when you attend an indoor dinner party, get a haircut, or go to the office. Your budget gets completely blown if you spend time in a crowd.
- Keep higher-risk activities as short as possible
- Follow the suggested instructions and safety measures put in place in your work environment
Fighting Covid-19 means giving the most effective treatment at the correct time. Our immune systems get weaker as we age and from higher glucose levels. With diabetes, a CGM is the most efficient way to monitor glucose levels and adjust insulin doses that may require rapid and substantial increases once an infection starts. Insulin remains the most effective way to maintain healthy glucose levels during a Covid-19 attack.